The cholesterol-lowering statin drug Lipitor has become the best-selling drug of all time, generating more than $140 billion in global sales. This class of drugs garnered so much enthusiasm in the medical community that some U.S. health authorities facetiously proposed they be added to the public water supply like fluoride is. One cardiology journal even offered the tongue-in-cheek suggestion for fast-food restaurants to offer “MacStatin” [sic] condiments along with ketchup packets to help neutralize the effects of unhealthy dietary choices.
What Are Statins and How Do They Work?
Statins are drugs that can lower cholesterol. They work by blocking a substance that our body requires to make cholesterol.
Are Statins Bad for You?
Although statins may be effective at lowering cholesterol and potentially helping to reduce the risk of heart disease and even stroke, they come with a host of possible side effects that may do much more harm than good.
What Possible Side Effects?
As I discuss in the video Who Should Take Statins?, muscle-related side effects from cholesterol-lowering statin drugs “are often severe enough [to make] patients stop taking [them]. Of course, these side effects could be coincidental or psychosomatic and nothing to do with the drug,” given that many clinical trials show such side effects are rare. Of course, it is also possible that studies funded by the drug companies themselves may under-report side effects. The bottom line is that there’s an urgent need to establish the true incidence of statin side effects.
Researchers have found that those taking statins are significantly more likely to develop type 2 diabetes than those randomized to placebo sugar pills. Why? We’re still not exactly sure, but statins may have the double-whammy effect of impairing insulin secretion from the pancreas, as well as diminishing insulin’s effectiveness by increasing insulin resistance.
Even short-term statin use may approximately “double the odds of developing diabetes and diabetic complications,” and increased risks may persist for years after stopping statins.
Who Should Take Statins?
How should you decide if a statin is right for you? “If you have a history of heart disease or stroke, taking a statin medication is recommended.” Period. Full stop. No discussion needed. However, if you don’t have any known cardiovascular disease, then the decision should be based on calculating your own personal risk, which you can easily do online if you know your cholesterol and blood pressure numbers, with the American College of Cardiology risk estimator or the Framingham risk profiler. (My favorite is the ACC estimator because it gives your current ten-year risk, as well as your lifetime risk.)
Under the current guidelines, if your ten-year risk is below 5 percent, unless there are extenuating circumstances, you should stick to diet, exercise, and smoking cessation to bring down your numbers. In contrast, if your ten-year risk hits or exceeds 20 percent, then the recommendation is to add a statin drug on top of making lifestyle modifications. Under 7.5 percent, the tendency is to stick with lifestyle changes unless there are risk-enhancing factors; above 7.5 percent, move towards adding drugs. What are the risk-enhancing factors to take into account when making the decision? A bad family history, really high LDL, metabolic syndrome, chronic kidney or inflammatory conditions, and persistently high triglycerides, C-reactive protein, or LP(a).
Relative Risk vs. Absolute Risk
One of the problems with communicating statin evidence to support shared decision-making is that most doctors have a poor understanding of concepts of risk, probability, and statistics, but that understanding is critical for preventive medicine. As discussed in my video Are Doctors Misleading Patients About Statin Risks and Benefits?, when doctors offer a cholesterol-lowering drug, they’re doing something quite different from treating a patient who is sick.
When drug companies say a statin reduces the risk of a heart attack by 36 percent, that’s the relative risk. In a large clinical study, 3 percent of patients not taking the statin drug had a heart attack within a certain amount of time, compared to 2 percent taking the drug. So, the drug dropped heart attack risk from about 3 percent to 2 percent, which is about a one-third drop—hence, the 36 percent reduced relative risk statistic. Another way to look at the change from 3 percent to 2 percent is that the absolute risk only dropped 1 percent. So, in effect, one’s chance of avoiding a heart attack over the next few years may be about 97 percent without treatment, but it can be increased to about 98 percent by taking daily statin drug. Yet another way to look at it: A hundred people would need to take the drug to prevent a single heart attack.
The Myth vs. the Reality
If you ask patients what they were led to believe, they think the chance of avoiding a heart attack within a few years on statins is 1 in 2, when it’s really 1 in a 100. And, if you ask, they want an absolute risk reduction of at least 30 percent or so to take a cholesterol-lowering drug every day, whereas the actual absolute risk reduction is only about 1 percent. So, the dirty little secret is that if patients knew the truth about how little these drugs actually worked, almost no one would agree to take them. So, doctors are either not educating their patients or they’re actively misinforming them.
Weighing the Risks and Benefits of Statins
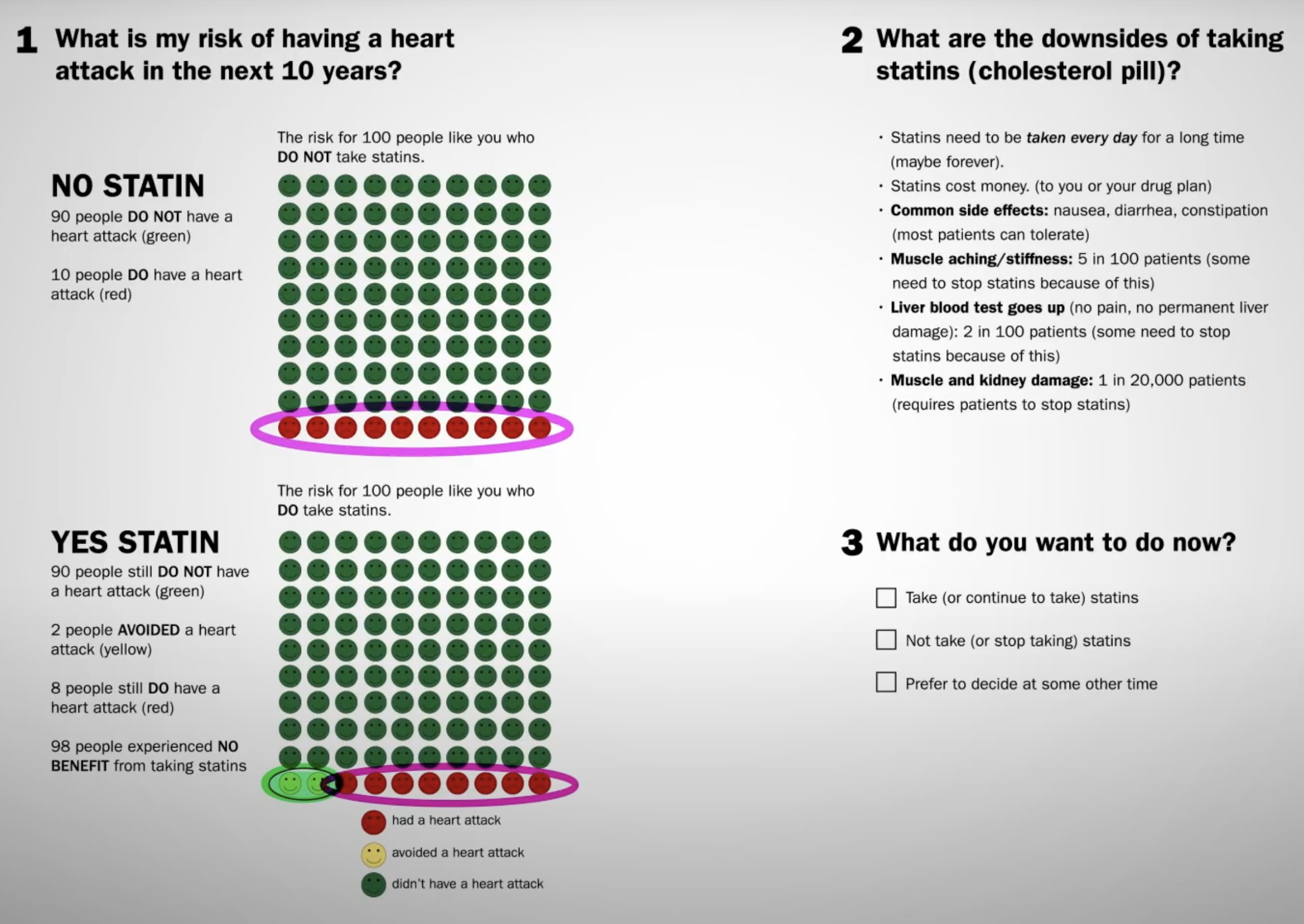
If all those numbers are blurring together, the Mayo Clinic developed a great visualization tool. For individuals at average risk who do not take a daily statin, 10 out of 100 may have a heart attack over the next ten years. However, if all 100 people took a statin every day for those ten years, 8 would have a heart attack and 2 would be spared. That’s about a 1 in 50 chance that taking the drug would help you avert a heart attack over the next decade. What if you have no known heart disease and you take statins for a few years? The chance statins will actually save your life is about 1 in 250.
What are the downsides? The cost and inconvenience of taking a pill every day, which can cause some gastrointestinal side effects, muscle aching and stiffness in maybe 5 percent, reversible liver inflammation in 2 percent, and more serious damage in perhaps 1 in 20,000 patients.
If you want a more personalized approach, calculate your ten-year risk. I cover this in more detail in my video The True Benefits vs. Side Effects of Statins.
Alternatives to Statins?
As I discuss in my video How Much Longer Do You Live on Statins?, taking statins can enable you to live years longer because, for every millimole per liter you drop your bad LDL cholesterol, you may live three or even six years longer, depending on which study you’re reading. A millimole in U.S. units (mg/dL) is 39 points. Drop your LDL cholesterol about 39 mg/dL or 1 mmol/L, and you could live years longer. Exercise your whole life, and you may only increase your lifespan by six months, whereas stopping smoking may net you nine months. So, how can you drop your LDL cholesterol by about 39 points? You can accomplish that by taking drugs every day, or you can achieve that within just two weeks of eating a diet packed with fruits, vegetables, and nuts.
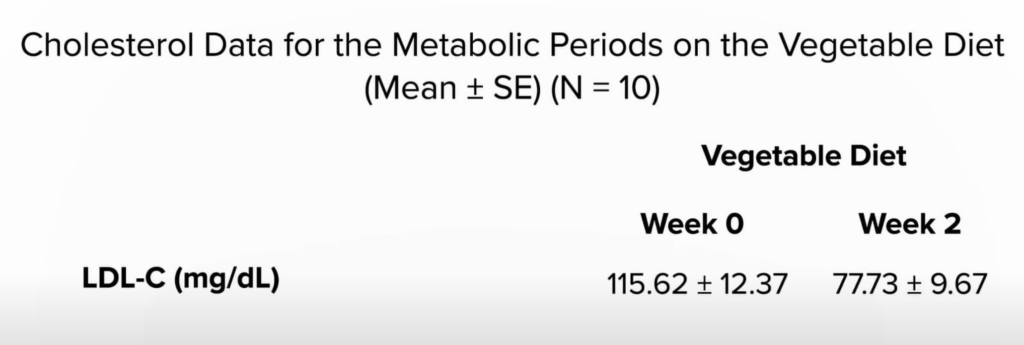
A plant-based diet has been shown to substantially reduce cholesterol levels and cardiovascular risk, as well as obesity, hypertension, and systemic inflammation—without negative side effects.







