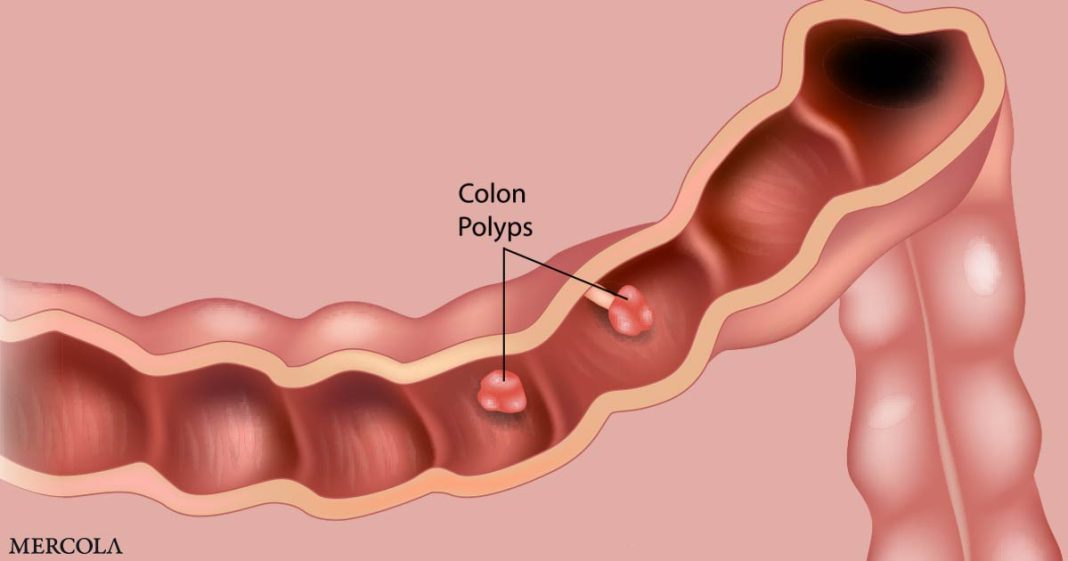
Going in for a routine checkup and hearing your doctor mention the word “polyps” sounds alarming, but understanding what colon polyps are and how to prevent them is important for optimal health. Colon polyps are abnormal growths that develop on the inner lining of your colon, which is part of your large intestine.
Think of your colon as a garden hose; polyps are like small bumps that form on the inside. While many polyps are harmless, some become cancerous over time, making early detection, symptom awareness and prevention important.
Symptoms of Colon Polyps
One of the trickiest things about colon polyps is that they often don’t cause any noticeable symptoms. Because symptoms are often absent, it’s easy to dismiss any subtle changes in your body. However, being aware of warning signs, even if they seem minor, is a first step in protecting your health.
While most polyps remain quiet, some trigger changes in your bowel habits. This includes persistent constipation, where you have difficulty passing stool, or the opposite, diarrhea, where you experience frequent, loose stools.
For example, if you normally have regular bowel movements and suddenly find yourself consistently constipated or experiencing diarrhea for more than a few days, it’s worth paying attention. These changes occur because larger polyps partially block your colon, interfering with the normal passage of waste. If you notice persistent changes in your bowel habits, it’s important to consult a doctor to determine the cause.
Another sign is rectal bleeding or blood in your stool. While blood in the stool is associated with other conditions as well, it’s important to take it seriously. Blood in the stool typically appears bright red or dark and tarry, depending on where the bleeding is occurring. Even if you don’t have any other symptoms, some polyps bleed intermittently.
Some people with colon polyps also experience abdominal discomfort, cramps or bloating.1 This manifests as a persistent ache, sharp pains or a feeling of fullness in your abdomen. Imagine a kink in a garden hose; it causes pressure to build up behind the kink.
Similarly, large polyps partially block your colon, leading to a buildup of gas and pressure, resulting in discomfort. It’s important to remember that these symptoms are not unique to colon polyps and are also caused by other digestive issues.
Common Risk Factors for Colon Polyps
Understanding the factors that contribute to the development of colon polyps is key to prevention. While some risk factors are beyond your control, such as age and genetics, others, like lifestyle choices, are not. Age is a significant factor in the development of colon polyps. Studies suggest that the prevalence of adenomas — a common type of polyp — increases with age, ranging from about 20% in people at age 45 to over 50% in those around 85 years old.2
Genetics also plays a role. Familial adenomatous polyposis (FAP) is a hereditary condition caused by a mutation in the APC gene. People with FAP develop numerous colon polyps and have a very high risk of developing colorectal cancer, often before the age of 40. This highlights the strong link between genetics and polyp development. If you have a family history of colon cancer or polyps, especially if diagnosed at a younger age, it’s important to discuss this with your doctor.
Several lifestyle factors also contribute to the risk of developing colon polyps, as mutations accumulate in your colon over time due to environmental factors including diet, lack of exercise and exposure to substances like pollution, tobacco and alcohol. A diet high in processed meats, for instance, contributes to polyp development, in part likely due to the generation of heterocyclic amines during cooking.3
Inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, also increases the risk of colon cancer. Chronic inflammation in your colon, a hallmark of IBD, promotes the formation of polyps.4
The Importance of Gut Health
The trillions of microorganisms residing in your gut, collectively known as your gut microbiota, play a key role in overall health, including your digestive health. Research increasingly suggests a strong link between the balance of these microorganisms and the development of colon polyps and colorectal cancer (CRC). A review published in the International Journal of Molecular Sciences highlights how disruptions in this balance, known as dysbiosis, contribute to these conditions.5
The study emphasizes that a healthy, fiber-rich diet is essential for maintaining a healthy gut microbiota. Regular fiber intake is recommended to maintain the integrity of your gut’s protective mucus layer and barrier function. When you don’t consume enough fiber, it leads to an increase in mucin-degrading bacteria and a decrease in the production of beneficial short-chain fatty acids (SCFAs). SCFAs have anti-inflammatory properties that help protect your colon.
However, avoiding high-fiber diets initially is important if your gut microbiome is compromised, as excessive fiber will increase endotoxin levels in this circumstance. So, if your gut health is severely compromised, focus on easily digestible carbohydrates like dextrose water for a week or two. Sip it slowly throughout the day to support gradual gut healing.
Next, try white rice and whole fruits to nourish beneficial bacteria before considering vegetables, whole grains and starches. These healthy carbohydrates play a role in supporting mitochondrial function since glucose is the preferred fuel for energy production at the cellular level. Tailor your carbohydrate consumption to support a healthy microbiome by aiming for 200 to 350 grams of targeted carbohydrates daily for most adults.
Conversely, a diet high in processed foods, unhealthy fat, refined sugar and alcohol negatively impacts your gut microbiota, increasing the risk of CRC, which often develops from adenomatous colon polyps. In addition to avoiding processed meats, it’s important to avoid seed oils, which are rich in linoleic acid that damages your gut microbiome and promotes harmful bacteria.
LA is a mitochondrial poison that compromises your cellular energy production, limiting your ability to maintain a healthy gut environment. In addition to processed foods, avoid nuts and seeds as well to reduce LA intake. It’s also advisable to avoid dining out, since most restaurants use seed oils in their cooking, sauces and dressings. Additionally, limit your consumption of chicken and pork, which are typically high in LA.
Replace processed foods with whole, unprocessed foods and healthy fats such as grass fed butter, tallow and ghee. It’s wise to keep your LA intake below 5 grams from all sources. If you can get it below 2 grams, that’s even better.
To help track your LA intake, enter all your daily meals into an online nutrition tracker. While more research is needed to fully understand the complex interactions between your gut microbiota and colon polyps, the evidence suggests that paying attention to gut health is a valuable part of a comprehensive prevention strategy.
Should You Get a Colonoscopy?
Colonoscopy is considered the gold standard for conventional colon cancer screening. During this procedure, a long, flexible tube with a camera is inserted into the rectum, allowing doctors to visualize the entire colon. The advantage of colonoscopy is that polyps are removed during the procedure. However, colonoscopy is an invasive procedure and carries risks.
For those at high risk, colonoscopies are sometimes useful, but it’s important to weigh the benefits against the harms, which include a risk of death. One analysis found a death rate of 3 per 100,000 colonoscopies, along with serious adverse events in 44 per 10,000, “with a number needed to harm of 225.”6 Other risks include bleeding after removal of a precancerous polyp and perforation.
Dysbiosis and other gut imbalances, caused by the process of flushing out your intestinal tract with harsh laxatives before the procedure, are another concern. How well the colonoscopy equipment is sterilized between patients also affects the riskiness of the procedure.
If you do choose to get a colonoscopy, it’s important to find a clinic or hospital that uses peracetic acid, which is similar to vinegar, to thoroughly sterilize the equipment by dissolving proteins found in the flexible endoscopes. Before scheduling any endoscopic examination call to ask how the equipment is sterilized between patients.
Several other screening options are also available, including the guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT), which check for the presence of blood or antibodies in your stool. There’s also a FIT-DNA test, sometimes called the stool DNA test, which combines FIT with a test to look for altered DNA in your stool.7
Flexible sigmoidoscopy and computed tomography (CT) colonography, also called virtual colonoscopy, are additional options. Flexible sigmoidoscopy is similar to a colonoscopy but uses a shorter and smaller scope, so it cannot see as far up into your colon. Many doctors fail to review the benefits and risks of each screening option with their patients, however, and instead only recommend colonoscopy.
Protecting Your Colon Health Using a Proactive Approach
Colon polyps are often silent, but they don’t have to be a threat to your future health. By understanding the symptoms, knowing your risk factors and adopting healthy lifestyle habits, you significantly reduce your risk. A healthy diet that eliminates processed food, regular exercise and maintaining a healthy weight are among your best natural defenses.
In addition, exposure to synthetic endocrine-disrupting chemicals (EDCs), estrogen and pervasive electromagnetic fields (EMFs) further impair your cells’ ability to generate energy efficiently. This energy deficit makes it challenging to sustain the oxygen-free gut environment necessary for beneficial bacteria like Akkermansia to flourish.
Akkermansia is essential for a healthy microbiome, however, it’s important to eliminate all seed oils from your diet for at least six months before starting an Akkermansia supplementation program.
This preparatory period allows your body to recover mitochondrial function and create a more hospitable environment in your colon for the beneficial bacteria. By taking these steps, you maximize the benefits of Akkermansia supplementation and support overall gut health.
When selecting Akkermansia supplements, choose those that utilize advanced, timed-release capsules or microencapsulation technology. These methods keep the bacteria dormant and protected until they reach your colon, typically within two to four hours after ingestion, ensuring that a higher number of live bacteria survive the journey through your digestive system. In addition, antibiotics devastate beneficial gut bacteria and significantly increase your risk of colon cancer.
Use antibiotics only when absolutely necessary and focus on rebuilding gut flora through targeted dietary choices, including fermented foods, afterward. Also avoid conventionally raised meats that typically contain antibiotic residues by choosing high-quality, responsibly sourced proteins to support a healthy microbiome. By taking a proactive approach to your health, you significantly reduce your risk of developing colon polyps and colon cancer and ensure a healthier future.